For months, if not years, I had been having trouble sleeping. I would wake up several times during the night and could not fall back to sleep. I got up to go the bathroom at least twice every night. Sometimes I was sweaty, sometimes cold. In the morning I did not feel refreshed; I was still tired and didn’t want to get out of bed. I would get very sleepy driving to and from work. I was told that I snored…but I didn’t believe it!
I finally discussed my sleep difficulties with my physician. She suggested that I try Melatonin which is available over the counter. That wasn’t successful so then we tried prescription sleep aids. These would definitely help me fall asleep, but I wouldn’t stay asleep. Still, I would awaken during the night and felt tired the next day. The effects of using some of the sleep aids, was worse than not taking anything at all. I was so groggy the next day I could hardly function for an hour or so.
Then, she suggested that I have a sleep study. I thought about it, but I wasn’t too keen on the idea. I kept trying the pills until I got fed up. Then we scheduled the sleep study.
You report to a sleep laboratory late in the evening, around 8:30pm. The sleep laboratory looked like a doctor’s office, but the examining room was just like a hotel bedroom! Weird!
You slip into your jammies and then they attach sensors to your legs, arms, chest and a whole bunch on your face and on your scalp. They use some gunk to make them stick that gets all stuck in your hair. They also put an oxygen sensor on your finger so they can monitor your oxygen level.
Once you are all wired up, you slip into bed and the technician leaves the room and talks to you through a speaker from a control booth. They run you through a series of movements to make sure the sensors are working. Things like: raise your right leg…raise your left leg…cough, etc. Nothing they put on you shocks you or hurts in any way. It just feels weird to be connected to all the wires.
So I laid there and watched TV until I got sleepy…not easy in a strange environment. They say I fell asleep but I didn’t believe it. I kept tossing and turning and waking up. The technician would come in from time to time to check on things. At 5:00am they wake you up and send you home. That concluded Part I of the study. The results were sent to my doctor in a few days. Evidently, I stopped breathing several times during the night for brief periods (apnea), or was breathing too shallow when I slept. This causes a condition called hypoxia, which basically too little oxygen getting to the brain. Your body is smart…it wakes you up so you can breathe and get oxygen. So that was the vicious cycle I was caught up in.
It seems that I had a case of Obstructive Sleep Apnea. Causes of sleep apnea include obesity, asthma, GERD, and lifestyle choices. No matter what the cause, the results are the same: the throat collapses or becomes obstructed, causing breathing to stop for several seconds, disrupting sleep. This explained my excessive daytime sleepiness, feeling tired, snoring, problems with concentration, morning headaches and nocturia.
Sleep apnea and obesity have an interrelated relationship. There is little doubt in the medical community that excess weight can cause sleep apnea: the extra fat and soft tissue in the throat puts pressure on the airway, increasing the chance that the airway passage will collapse. Sixty to seventy percent of sleep apnea patients are obese.
While obesity is a cause of sleep apnea, the relationship between sleep apnea and obesity is even more complex. Additional weight gain is a common sleep apnea symptom, so obesity can cause sleep apnea, and sleep apnea in turn can worsen obesity.
A few days later, the lab called me to come back for Part 2 of the Sleep Study…almost the same thing, but this time they would fit me with a face mask and have me on an Apnea monitor. Sometimes, they do this is one session, but for me, they did it in two separate sessions.
The apnea monitor delivers pressurized oxygen via a face mask. They increase the pressure little by little until your oxygen levels are within an acceptable range. It was a uncomfortable trying to sleep with a mask on my face. They told me I had to keep using it and would eventually get used to it. Ha! I decided to go along with it, as I was desperate for a good night’s sleep.
The results of Part 2 of the sleep study identified my problem and a prescription was written for an apnea monitor for me to use at home. A medical supply company sends a representative to deliver the device, set it up and show you how to use it.
To be honest, compliance was difficult. Some nights I just didn’t want some device on my face. But when I started seeing improvement in my sleep, I was encouraged to keep using it.
The fact that I was diagnosed with obstructive sleep apnea was a factor in qualifying me for weight loss surgery. Who knew?
Statistics show that people are trying to lose weight either through medically supervised diet programs, commercially operated programs, or fad diets. The success dieters experience varies greatly depending on starting weight, diet method, and length of diet. Some dieters do achieve and maintain a reduced body weight, although not necessarily their goal weight. The sad truth is that the majority of dieters regain all of the weight they lost —and sometimes even more — within two to five years.
For unsuccessful dieters, each pound regained will take its toll in personal frustration and an overwhelming sense of failure. For the severely obese the toll of those regained pounds may be especially high.
One of the reasons I decided to look into weight loss surgery was because I had indeed developed some of these conditions. Before I knew it, I was on medication I had to take twice a day. I felt like I was a sick person and I didn’t like that feeling at all.
Because of the failure of most diet programs to bring about permanent weight loss, and because of the serious physical, psychological, social, and economic consequences of severe obesity, the medical community has been working to develop diet programs that really work.
Overweight is defined as an excess body weight. Muscle, bone, fat and/or body water may contribute to excess weight. However, obesity is defined as an excess of body fat. From a medical perspective, those who are obese are suffering from a kind of physical illness, or at an increased risk for developing an illness.
According to the Center for Disease Control (CDC), the incidence of obesity in the United States has increased over time. Nearly one-third of adults over the age of twenty have a BMI of or higher than 30. In the past 30 years the rate of obesity has nearly tripled for children (ages two to five) and adolescents (ages twelve to nineteen). Alarmingly, obesity has quadrupled for children ages six to eleven. Because of these increases, obesity is considered to be a public health crisis. The reason for concern is the fact that obesity contributes to, or makes worse, a number of illnesses. An obese person may suffer from one or more of the following conditions:
- An overworked heart and circulatory system
- Shortness of breath
- High Blood Pressure
- Diabetes
- Poor capacity for physical activity
- Strain on joints and ligaments resulting in pain
- Poor adjustment to temperature change
- Increased susceptibility to infectious disease
- Psychological and social problems due to an obese appearance
Most importantly, medical evidence shows that being overweight may shorten your life span. Well, when that though finally registered in my brain, I knew it was time to take action. I wanted to cure my “disease” and live a normal, healthy, long life. So, thus my weight loss journey began.
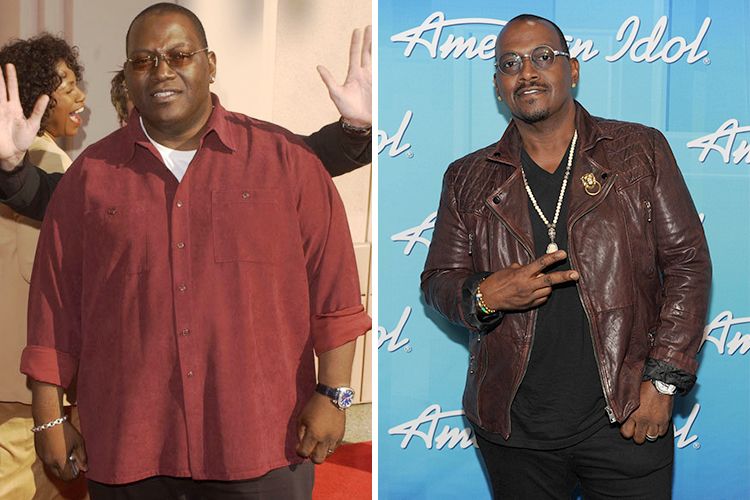
When I visited the doctor for my consultation in November 2014, I weighed in at 238 pounds. I had RNY gastric bypass surgery on May 19, 2015. Today, I am 171 lbs and no longer take any medication other than my vitamins and supplements. I am wearing a size 10 in pants (previously a size 18-20) and no longer need to shop at the “plus size” stores. I am experiencing a weight loss plateau (not losing but not gaining) for about three weeks, but I know all the reasons why. Too many carbs and not enough exercise. The surgery can fix your body and give you a tool to help you lose the weight, but only you can fix your mind. After the surgery, you still need to make good food choices. I know I will have this struggle for the rest of my life.
Weight Loss Surgery: Which Type Should You Have?
Surgical procedures use two basic methods to cause weight loss: Restriction and/or Malabsorption.
Restriction limits how much food you can eat at one time. This is done by making a portion of your stomach smaller so it holds less food. This way, you feel full after eating a small amount.
Malabsorption limits how much food your body absorbs. This is done by shortening the small intestine so that food only travels through a short section. The result is that most of the food eaten is expelled as waste and not absorbed as energy.
What I learned is that the LAP-BAND® is only a restrictive procedure. Also, it is meant to be permanent, not temporary. It also requires regular office visits to have “fills”. There is a port just under your skin by your tummy, where your surgeon inserts a needle to fill the LAP-BAND® with saline solution to tighten the band every so often.
This may work well for many people, but as my surgeon explained, I needed to examine my own eating habits. If sweets and fats are my weakness, then I may benefit from a procedure that is both restrictive and malabsorptive. Food for thought. How did he know cookies were my weakness?
RNY Surgery (Roux-en-Y Gastric Bypass)
The Roux-en-Y Gastric Bypass procedure (RNY Surgey) is considered, by some, as the “gold standard” in bariatric surgery. It is both restrictive and malabsorptive. As such, it comes with a built-in deterrent called “dumping syndrome”.
Dumping syndrome occurs when a large load of simple carbohydrates (such as table sugar, syrups, honey, ice cream, sugary desserts, candies, cookies, sweet drinks) enter the small intestine too quickly after eating.
This may result in all or some of the following symptoms: Abdominal fullness/bloating, nausea, or cramping followed by diarrhea. Other symptoms include fatigue, increased heart rate, cold sweats, felling warm/flushed, dizzy, weak, or faint. To avoid dumping, all you need to do is avoid simple carbohydrates!
After giving it some thought, and analyzing my eating patterns, I thought I would need more than just a restrictive procedure. If I did the surgery, I wanted the best possible outcome and long term weight control.
I attended support groups for both LAP-BAND® and Gastric Bypass patients. Both groups sung the praises of each and told of their successes. In the end, I chose to have Roux-en-Y Gastric Bypass surgery…and I’m glad I did.

